Select a tab to learn more about it
Nearsightedness (myopia) is a common vision condition in which you can see objects near to you clearly, but objects farther away are blurry.
The degree of your nearsightedness determines your ability to focus on distant objects. People with severe nearsightedness can see clearly only objects just a few inches away, while those with mild nearsightedness may clearly see objects several yards away.
Nearsightedness may develop gradually or rapidly, often worsening during childhood and adolescence. Nearsightedness tends to run in families.
A basic eye exam can confirm nearsightedness. You can easily correct the condition with eyeglasses or contact lenses.
Farsightedness (hyperopia) is a common vision condition in which you can see distant objects clearly, but objects nearby may be blurry.
The degree of your farsightedness determines your focusing ability. People with severe farsightedness may see near objects less clearly than distant objects, while those with mild farsightedness may be able to clearly see objects that are closer.
Farsightedness usually is present at birth and tends to run in families. You can easily correct this condition with eyeglasses or contact lenses.
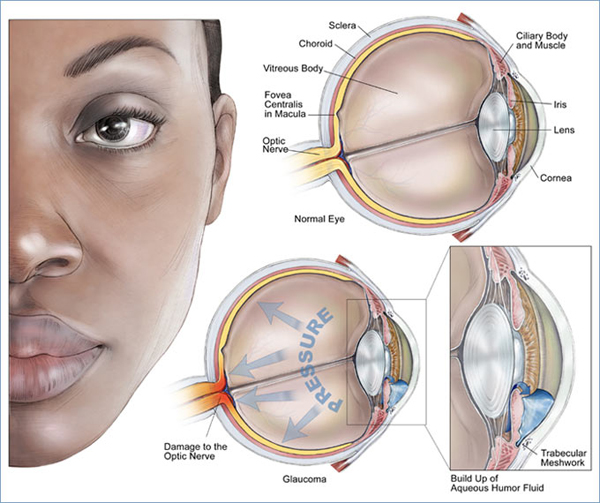
Glaucoma is not just one eye disease, but a group of eye conditions resulting in optic nerve damage, which causes loss of vision. Abnormally high pressure inside your eye (intraocular pressure) usually, but not always, causes this damage.
Glaucoma is the second leading cause of blindness. Sometimes called the silent thief of sight, glaucoma can damage your vision so gradually you may not notice any loss of vision until the disease is at an advanced stage. The most common type of glaucoma, primary open-angle glaucoma, often has no noticeable signs or symptoms.
Early diagnosis and treatment can minimize or prevent optic nerve damage and limit glaucoma-related vision loss. It's important to get your eyes examined regularly, and make sure your eye doctor measures your intraocular pressure.
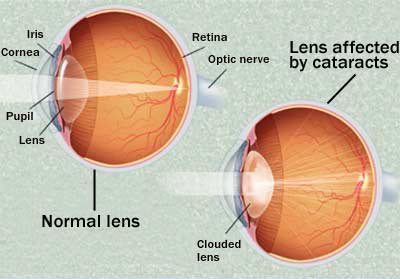
A cataract is a clouding of the normally clear lens of your eye. For people who have cataracts, seeing through cloudy lenses is a bit like looking through a frosty or fogged-up window. Clouded vision caused by cataracts can make it more difficult to read, drive a car, especially at night, or see the expression on a friend's face.
Most cataracts develop slowly and don't disturb your eyesight early on. But with time, cataracts will eventually interfere with your vision.
At first, stronger lighting and eyeglasses can help you deal with cataracts. But if impaired vision interferes with your usual activities, you might need cataract surgery. Fortunately, cataract surgery is generally a safe, effective procedure.
What Is Astigmatism?
Astigmatism is a common eye condition that's easily corrected by eyeglasses, contact lenses, or surgery. Astigmatism is characterized by an irregular curvature of the cornea. This is one type of refractive error. Astigmatism occurs in nearly everybody to some degree. For significant curvature, treatment is required.
A person's eye is naturally spherical in shape. Under normal circumstances, when light enters the eye, it refracts evenly, creating a clear view of the object. However, the eye of a person with astigmatism is shaped more like a football or the back of a spoon. For this person, when light enters the eye it is refracted more in one direction than the other, allowing only part of the object to be in focus at one time. Objects at any distance can appear blurry and wavy.
What Causes Astigmatism?
Astigmatism can be hereditary and is often present at birth. It can also result from pressure from the eyelids on the cornea, incorrect posture, or an increased use of the eyes for close work.
What Are the Symptoms of Astigmatism?
People with undetected astigmatism often experience headaches, fatigue, eyestrain, and blurred vision at all distances. While these symptoms may not necessarily be the result of astigmatism, you should schedule an eye exam if you are experiencing one or more symptoms.
How Are Astigmatisms Diagnosed?
Your optometrist or Optician can diagnose astigmatism with a thorough eye exam. Astigmatism may occur with other refractive errors such as myopia ( nearsightedness) and hyperopia ( farsightedness). Unfortunately, astigmatism often goes undetected in school-age children.
Because astigmatisms may increase slowly, you should visit your optometrist or Optician whenever you notice significant changes in your vision. Optometrists are trained specifically to examine the general health of the eyes and prescribe eyeglasses and contact lenses. Opticians provide total eye care, including exams, diagnosis, and treatment of disease through medication and surgery.
How Are Astigmatisms Treated?
Almost all degrees of astigmatism can be corrected with properly prescribed eyeglasses or contact lenses. For a person with only a slight degree of astigmatism, corrective lenses may not be needed at all, as long as other conditions such as nearsightedness or farsightedness are not present. If the astigmatism is moderate to high, however, corrective lenses are probably needed.
Corrective lenses (eyeglasses or contact lenses):
For astigmatism, special corrective lenses called toric lenses are prescribed. Toric lenses have greater light bending power in one direction than the other. After performing various tests, your eye doctor will determine the ideal toric lens prescription for your astigmatism.
Refractive surgery.
Another method for correcting astigmatism is by changing the shape of the cornea through refractive or laser eye surgery. While there is more than one type of refractive surgery, specific treatments are recommended on an individual basis.
Refractive surgeries require healthy eyes that are free from retinal problems, corneal scars, and any eye disease. As technology progresses, it is becoming more and more important that you explore all options and possibilities before deciding which refractive surgery and treatment is right for you.
The gradual loss of your eyes' ability to focus actively on nearby objects is a not-so-subtle reminder that you've reached middle age. A natural, often annoying part of aging, presbyopia usually becomes noticeable in your early to mid-40s and continues to worsen until around age 65. You may become aware of presbyopia when you start holding books and newspapers at arm's length to be able to read them. If you're nearsighted, you might temporarily manage presbyopia by reading without your glasses. A basic eye exam can confirm presbyopia. You can correct the condition with prescription eyeglasses.
Amblyopia, commonly known as lazy eye, is a condition where vision in one of the eyes is reduced because the eye and the brain are not working together properly. The visual loss in amblyopia cannot be corrected by just wearing glasses. Amblyopia is the most common cause of visual impairment during childhood. The condition affects approximately 2 to 3 out of every 100 children. It is thought to develop early in life during the critical period of visual development. Unless it is successfully treated in early childhood, amblyopia usually persists into adulthood, and is the most common cause of monocular (one eye) visual impairment among children and young and middle-aged adults.
What causes amblyopia?
Amblyopia may be caused by any condition that affects normal visual development or use of the eyes. Strabismus, which is an imbalance in the positioning of the two eyes, is the most common cause of amblyopia. Strabismus can cause the eyes to cross in (esotropia) or turn out (exotropia). Other causes of amblyopia include childhood cataracts, nearsightedness, farsightedness and astigmatism. There is often a family history of this condition.
What are the symptoms of amblyopia?
The symptoms of amblyopia include:
- Eyes that turn in or out
- Eyes that do not appear to work together
- Inability to judge depth correctly
- Poor vision in one eye
How is amblyopia diagnosed?
Amblyopia is usually easily diagnosed with a complete examination of the eyes. Special tests are usually not needed.
What is he treatment for amblyopia?
In general, the earlier the child has the condition for the development of amblyopia the worse it may become. Similarly, the earlier the treatment is started, the better the opportunity to reverse vision loss. Before treating amblyopia, it may be necessary to first treat the underlying cause. Glasses are commonly prescribed to improve focusing or misalignment of the eyes. Surgery may be performed on the eye muscles to straighten the eyes if non-surgical means are unsuccessful. Surgery can help in the treatment of amblyopia by allowing the eyes to work together better. Eye exercises may also be recommended either before or after surgery to correct faulty visual habits associated with strabismus and to teach comfortable use of the eyes. Following treatment of the underlying cause, patching or covering one eye may be required for a period of time. The better-seeing eye is patched, forcing the “lazy” one to work, thereby strengthening its vision. Eye drops or ointment may also be used to blur the vision of the good eye in order to force the weaker one to work. This method, however, is generally a less successful approach.
Keratoconus is an eye condition in which the shape of the cornea becomes distorted. The cornea is a clear structure that covers the front of the eye and allows light to enter the eye. In a healthy eye, the cornea curves like a dome. In an eye with keratoconus, the center of the cornea slowly thins and bulges so that it sags and has a cone shape.
What causes keratoconus?
The cause of keratoconus is unknown.
What are the symptoms of keratoconus?
Keratoconus tends to affect younger people and the symptoms sometimes start in the early teen years and progresses most rapidly for the next 10 to 20 years. Often, eyeglass prescriptions must be changed frequently as the disease progresses.
Symptoms include:
- Difficulty driving at night
- Halo's and ghosting, especially at night
- Eye strain
- Headaches and general eye pain
- Eye irritation and excessive rubbing of the eye
How is keratoconus diagnosed?
Keratoconus can usually be diagnosed with a slit-lamp examination as well measurement of the corneal curvature. Your optometrist will look for signs such as corneal thinning, stress lines, and scarring at the apex of the corneal cone. Keratoconus, especially in the early stages, can be difficult to diagnose and its symptoms could be associated with other eye problems. Simply recognizing symptoms does not by itself diagnose the condition.
What is the treatment for keratoconus?
The primary treatment options for keratoconus are contact lenses and surgery. In the very early stages of keratoconus, vision problems can be corrected with prescription glasses or contact lenses. As keratoconus progresses, special rigid gas permeable contact lenses may be necessary. Advanced keratoconus may require surgery.
The term “macular degeneration” includes many different eye diseases, all of which affect central, or detail vision. Age-related macular degeneration is the most common of these disorders, mainly affecting people over the age of 60. Although there are many types of macular degeneration, age-related macular degeneration (AMD or ARMD) is the most common type. Age-related macular degeneration occurs in two forms: “wet” age-related macular degeneration and “dry” age-related macular degeneration. “Wet” age-related macular degeneration is less common but more aggressive in its development to severe central vision loss. “Dry” age-related macular degeneration is the more common type and is more slowly progressive in causing loss of vision.
What is wet age-related macular degeneration?
Wet age-related macular degeneration occurs when abnormal blood vessels begin to grow underneath the retina. These new blood vessels (known as choroidal neovascularization or CNV) tend to be very fragile and often leak blood and fluid. The blood and fluid raise the macula from its normal place at the back of the eye and interfere with the retina's function and causes the central vision to blur. Under these circumstances, vision loss may be rapid and severe. Some patients, however, do not notice visual changes despite the onset of CNV. Therefore, periodic eye examinations are very important for patients at risk for CNV. Once CNV has developed in one eye, whether there is a visual loss or not, the other eye is at relatively high risk for the same change.
What is dry age-related macular degeneration?
In dry AMD, the light-sensitive cells in the macula slowly break down. With less of the macula functioning, central vision diminishes. Dry AMD often occurs in just one eye at first. Later, the other eye can be affected. The cause of dry AMD is unknown. The dry form is much more common than the wet form. Dry AMD can advance and cause vision loss without turning into wet AMD. Dry AMD can also rapidly transform into the wet form by the growth of new blood vessels.
What causes macular degeneration?
We do not know the precise cause for the development of ARMD. However, we do know that there are certain risk factors for the development of age-related macular degeneration.
What are risk factors for macular degeneration?
The greatest risk factor is age. Although AMD may occur during middle age, studies show that people over age 60 are clearly at greater risk than other age groups.
What are the symptoms of macular degeneration?
Neither dry nor wet AMD cause any eye pain. The most common early symptom in dry AMD is blurred vision. Dry macular degeneration symptoms usually develop gradually and do not include total blindness. However, the symptoms may worsen the quality of life by making reading, driving, and facial recognition difficult. Other symptoms may include decreased night vision, a decrease in the intensity or brightness of colors, increase in the haziness of overall vision. All of the above symptoms may also be noticed in the wet form of AMD. In addition, the most common symptom in wet macular degeneration is straight lines appearing crooked or wavy.
How is macular degeneration diagnosed?
A thorough examination by an eye doctor is the best way to determine if you have macular degeneration or if you are at risk for developing the condition. The exam begins by testing your visual acuity or the sharpness of your vision. There are several different tests for visual acuity. The most familiar one has lines of black letters on a white chart. Next, your eyes may be tested with an Amsler grid. This test helps your doctor determine if you are experiencing areas of distorted or reduced vision, both common symptoms of macular degeneration. If you do have macular degeneration, your doctor will use the Amsler grid to determine if your vision has changed. After these visual tests, the front part of your eyes will be examined to determine if everything is healthy. Your doctor may put anesthetic drops in your eyes before measuring the pressure in each eye. Drops are also administered, which cause your pupils to dilate. This will allow your doctor to examine the retina through the enlarged pupil. After the dilating drops are administered and allowed time to work, the eye doctor will then use a slit-lamp to examine the eyes. The slit-lamp is a special microscope that enables the doctor to examine the different parts of the eye under magnification. When used with handheld lenses or special contact lenses, the slit-lamp gives the examiner a highly magnified view of the retina.
What is the treatment for wet macular degeneration?
Wet AMD can be treated with laser surgery, photodynamic therapy, and injections into the eye. None of these treatments is a permanent cure for wet AMD. The disease and loss of vision may continue to grow despite treatment.
What is the treatment for dry macular degeneration?
There is currently no treatment available to reverse dry macular degeneration. However, dry macular degeneration usually develops at a slower pace and most patients with this condition are able to live relatively normal, productive lives. Often one eye is affected more than the other.
If you have been diagnosed with diabetes, you may be at risk of losing your vision since your body does not utilize sugar properly and, when the sugar levels rise, damage to the retinal blood vessels may occur. This injury to the retinal vessels is known as Diabetic Retinopathy. Diabetic Retinopathy is the leading cause of blindness in working-age adults.
What are the symptoms of diabetic retinopathy?
Often, one may not be aware of any symptoms even when significant diabetic retinopathy is present. When macular edema occurs, vision often becomes blurry and may fluctuate. If abnormal new blood vessels form, as in proliferative diabetic retinopathy, they may bleed and result in small specks or large floaters obscuring the vision. If a large hemorrhage occurs, vision often becomes very blurry.
How is diabetic retinopathy diagnosed?
A comprehensive eye examination by an optometrist or retina specialist is the only reliable means of detecting diabetic retinopathy. After the pupil is dilated, a device called an ophthalmoscope is used to view the retina and determine the extent of the retinopathy. If diabetic retinopathy is discovered, a fluorescein dye test and/or optical coherence tomogram (OCT) may be recommended. A fluorescein angiogram involves the injection of a dye into a vein in the arm followed by several minutes of intermittent photos with a special digital camera focused on the retina. An OCT is a non-invasive photo that creates a detailed cross-sectional image of the macula.
What is the treatment for diabetic retinopathy?
The best therapy for diabetic retinopathy is prevention. Studies show that strict control of blood sugar levels can significantly lower the risk of vision loss from diabetic retinopathy. High blood pressure and kidney problems should also be treated to minimize their effect on the retinopathy. Laser surgery is often the first line of treatment if macular edema or proliferative retinopathy is present. For macular edema, the laser is focused on leaky areas of the retina to aid in reabsorbing the excess fluid. The primary goal of this treatment is to prevent further vision loss. It is uncommon for people to recover significant vision following treatment but some do experience partial restoration. Laser surgery is not a cure for diabetic retinopathy and is not guaranteed to prevent further loss of vision. Other treatments for diabetic retinopathy include medications like steroids or a novel class of medication called anti-VEGF.
Below are some of the most common eye infections associated with wearing contact lenses.
What is keratitis?
The most common infection related to contact lens use is keratitis, an infection of the cornea (the clear, round dome covering they eye's iris and pupil). Keratitis can be caused my many things, including herpes, bacteria, fungus and microbes. It is not transmitted from person to person, but fungal keratitis is more common in warmer climates.
What are the symptoms of keratitis?
Symptoms of keratitis may include:
- Blurry vision
- Unusual redness of the eye
- Pain in the eye
- Tearing
- Excessive tearing or discharge from your eye
- Increased light sensitivity
- Foreign body sensation
How is keratitis diagnosed and treated?
Keratitis can sometimes cause serious vision loss or even blindness, so it is important to see an optometrist if you are experiencing the above symptoms. Fungal keratitis is treated with topical and oral antifungal medications. Patients who do not respond to medical treatment may require eye surgery, possibly including a corneal transplant.
What are corneal ulcers?
A corneal ulcer is an erosion or exposed sore on the surface of the cornea. Corneal ulcers are most commonly caused by germs. Other causes of corneal ulcers include viruses, injury and inadequate eyelid closure. Corneal ulcers are common in people who wear contact lenses, especially if they wear them overnight.
What are the symptoms of corneal ulcers?
The symptoms of corneal ulcers include:
- Redness
- Pain
- Tearing
- Discharge
- White spot on the cornea
- Blurry vision
- Burning
- Itching
- Light sensitivity
How are corneal ulcers diagnosed and treated?
Early diagnosis is important in treating corneal ulcers. Your optometrist will ask you questions to determine what caused the ulcer. Your eyes will then be examined with a slit-lamp. A special dye may be placed in your eye to aid in the diagnosis. If it is not clear what the exact cause is, your optometrist may test a sample of the ulcer in order to properly treat it. Treatment for corneal ulcers needs to be aggressive, as some ulcers can lead to vision loss and blindness. Treatment usually involves antibiotics as well as antiviral or antifungal medications. Steroid eye drops may also be given to reduce inflammation. In severe cases, a corneal transplant may be needed to restore vision. If treatment is not administered, there may be blindness or even total loss of the eye.
What is Contact Lens Induced Acute Red Eye (CLARE)?
CLARE is an inflammatory reaction of the cornea and conjunctiva (a thin and transparent membrane that covers the sclera, the white part of the eye). This infection is mostly caused by sleeping with contact lenses and is characterized by awaking with red eyes.
What is the treatment for CLARE?
In most cases, no treatment is required. It is recommended that patients discontinue lens wear, which usually remedies the condition. However, if redness or irritation persists after 24 hours, you should see your optometrist. If you experience pain, sensitivity to light or decrease in vision, you should see your optometrist immediately.
What is Contact Lens Papillary Conjunctivitis (CLPC)?
CLPC is an inflammatory reaction of the upper eye lid and is very common among those that wear contact lenses.
What are the symptoms of CLPC?
The symptoms of CLPC include small, red bumps on the inflamed tissue on the underside of the upper eyelids. There is usually itchiness, discharge, increased lens awareness and decreased lens tolerance.
What is the treatment for CLPC?
Your optometrist may prescribe pharmaceutical eye drops such as anti-histamines and recommend that you stop wearing contacts until the condition goes away.
Strabismus (also called crossed eyes, deviation, heterotropia, squint, tropia) is a condition where both of your eyes do not look toward the same object together. There are six different muscles that surround the eyes and work together so that both eyes can focus on the same object. For someone with strabismus, these muscles do not work together. As a result, one eye looks at one object, while the other eye turns in a different direction and is focused on another object. When this happens, two different images, one from each eye, are sent to the brain. This confuses the brain, and the brain may learn to ignore the image from the weaker eye. Strabismus is a common condition among children but it can also occur later in life.
What are the symptoms of strabismus?
The main sign of strabismus is an eye that is not directed straight. Sometimes a child or young person will squint with one eye in bright sunlight. Symptoms of faulty depth perception may also be noticed. Adults with strabismus will usually have double vision.
How is strabismus diagnosed?
Strabismus is usually diagnosed with a physical examination that includes a detailed examination of the eyes. Tests are done to determine how much the eyes are out of alignment. These eye tests may include corneal light reflex, cover/uncover test, retinal exam, standard ophthalmic exam and visual acuity.
What is the treatment for strabismus?
Treatment of strabismus may consist of eyeglasses, patching, eye coordination exercises (called orthoptics) and/or surgery on the eye muscles. Eyeglasses, with or without patching, are often the treatment tried first and can usually reduce the amount of deviation.